

Diabetes also called Diabetes mellitus, is a term for several conditions involving how your body turns food into energy.
When you eat a carbohydrate, your body turns it into a sugar called glucose and sends that to your bloodstream. Your pancreas releases insulin, a hormone that helps move glucose from your blood into your cells, which use it for energy.
When you have diabetes and don’t get treatment, your body doesn’t use insulin like it should. Too much glucose stays in your blood, a condition usually called high blood sugar. This can cause health problems that may be serious or even life-threatening.
There’s no cure for diabetes. But with treatment and lifestyle changes, you can live a long, healthy life. Diabetes comes in different forms, depending on the cause.
million
people
million
people
%
people
.png)
.png)
Prediabetes is when your blood sugar is higher than it should be but not high enough for your doctor to diagnose diabetes. More than a third of people in the United States have it, but most of them don’t know it.
Prediabetes can make you more likely to get type 2 diabetes and heart disease . Exercising more and losing extra pounds, even as little as 5% to 7% of your body weight, can lower those risks.
Type 1 diabetes is also called insulin-dependent diabetes. It used to be called juvenile-onset diabetes, because it often begins in childhood.
Type 1 diabetes is an autoimmune condition. It happens when your body attacks your pancreas with antibodies. The organ is damaged and doesn't make insulin.
Your genes might cause this type of diabetes. It could also happen because of problems with cells in your pancreas that make insulin.
Many of the health problems that can come with type 1 happen because of damage to tiny blood vessels in your eyes (called diabetic retinopathy), nerves (diabetic neuropathy), and kidneys (diabetic nephropathy). People with type 1 also have a higher risk of heart disease and stroke.
Treatment for type 1 diabetes involves injecting insulin into the fatty tissue just under your skin.
You might use:
A test called the A1C blood test estimates your blood sugar levels over the previous three months. Your doctor uses it to see how well your blood sugar is controlled. That helps them know your risk of complications.
If you have type 1 diabetes, you’ll need to make changes including:
Type 2 diabetes used to be called non-insulin-dependent or adult-onset diabetes. But it’s become more common in children and teens over the past 20 years, largely because more young people are overweight or obese. About 90% of people with diabetes have type 2.
When you have type 2 diabetes, your pancreas usually creates some insulin. But either it’s not enough or your body doesn’t use it like it should. Insulin resistance, when your cells don’t respond to insulin, usually happens in fat, liver, and muscle cells.
Type 2 diabetes is often milder than type 1. But it can still cause major health complications, especially in the tiny blood vessels in your kidneys, nerves, and eyes. Type 2 also raises your risk of heart disease and stroke.
People who are obese -- more than 20% over their target body weight for their height -- have an especially high risk of type 2 diabetes and the health problems that can follow. Obesity often causes insulin resistance, so your pancreas has to work harder to make more insulin. But it’s still not enough to keep your blood sugar levels where they should be.
Treatment for type 2 diabetes involves keeping a healthy weight, eating right, and exercising. Some people need medication, too.
Your doctor might do an A1C test a few times a year to see how well you’ve been controlling your blood sugar.
Pregnancy usually causes some form of insulin resistance. If this becomes diabetes, it’s called gestational. Doctors often spot it in middle or late pregnancy. Because a woman’s blood sugars travel through their placenta to the baby, it’s important to control gestational diabetes to protect the baby's growth and development.
Doctors report gestational diabetes in 2% to 10% of pregnancies. It usually goes away after birth. But up to 10% of women who have gestational diabetes get type 2, weeks or even years later.
Gestational diabetes is more of a risk for the baby than the mother. A baby might have unusual weight gain before birth, trouble breathing at birth, or a higher risk of obesity and diabetes later in life. The mother might need a cesarean section because of an overly large baby, or they might have damage to their heart, kidney, nerves, and eyes.
Gestational diabetes treatment involves:
In 1% to 5% of people who have diabetes, other conditions might be the cause. These include diseases of the pancreas, certain surgeries and medications, and infections. In these cases, your doctor might want to keep an eye on your blood sugar levels.
Diabetes symptoms depend on how high your blood sugar is. Some people, especially if they have Prediabetes, gestational diabetes or type 2 diabetes, may not have symptoms. In type 1 diabetes, symptoms tend to come on quickly and be more severe.
Some of the symptoms of type 1 diabetes and type 2 diabetes are:
Type 1 diabetes can start at any age. But it often starts during childhood or teen years. Type 2 diabetes, the more common type, can develop at any age. Type 2 diabetes is more common in people older than 40. But type 2 diabetes in children is increasing.

Insulin is a hormone that comes from a gland behind and below the stomach (pancreas).

Glucose — a sugar — is a source of energy for the cells that make up muscles and other tissues.
The exact cause of most types of diabetes is unknown. In all cases, sugar builds up in the bloodstream. This is because the pancreas doesn't produce enough insulin. Both type 1 and type 2 diabetes may be caused by a combination of genetic or environmental factors. It is unclear what those factors may be.
Risk factors for diabetes depend on the type of diabetes. Family history may play a part in all types. Environmental factors and geography can add to the risk of type 1 diabetes.
Sometimes family members of people with type 1 diabetes are tested for the presence of diabetes immune system cells (autoantibodies). If you have these autoantibodies, you have an increased risk of developing type 1 diabetes. But not everyone who has these autoantibodies develops diabetes.
Race or ethnicity also may raise your risk of developing type 2 diabetes. Although it's unclear why, certain people — including Black, Hispanic, American Indian and Asian American people — are at higher risk.
Prediabetes, type 2 diabetes and gestational diabetes are more common in people who are overweight or obese.
Long-term complications of diabetes develop gradually. The longer you have diabetes — and the less controlled your blood sugar — the higher the risk of complications. Eventually, diabetes complications may be disabling or even life-threatening. In fact, Prediabetes can lead to type 2 diabetes. Possible complications include:
Diabetes majorly increases the risk of many heart problems. These can include coronary artery disease with chest pain (angina), heart attack, stroke and narrowing of arteries (atherosclerosis). If you have diabetes, you're more likely to have heart disease or stroke .
Too much sugar can injure the walls of the tiny blood vessels (capillaries) that nourish the nerves, especially in the legs. This can cause tingling, numbness, burning or pain that usually begins at the tips of the toes or fingers and gradually spreads upward. Damage to the nerves related to digestion can cause problems with nausea, vomiting, diarrhea or constipation. For men, it may lead to erectile dysfunction..

The kidneys hold millions of tiny blood vessel clusters (glomeruli) that filter waste from the blood. Diabetes can damage this delicate filtering system.
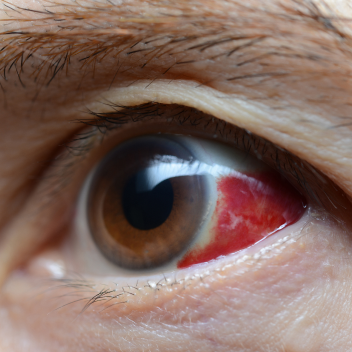
Diabetes can damage the blood vessels of the eye. This could lead to blindness.

Nerve damage in the feet or poor blood flow to the feet increases the risk of many foot complications.

Diabetes may leave you more prone to skin problems, including bacterial and fungal infections.

Hearing problems are more common in people with diabetes.
Type 2 diabetes may increase the risk of dementia, such as Alzheimer's disease.

Depression symptoms are common in people with type 1 and type 2 diabetes.
Most women who have gestational diabetes deliver healthy babies. However, untreated or uncontrolled blood sugar levels can cause problems for you and your baby.
Depression symptoms are common in people with type 1 and type 2 diabetes. can be caused by gestational diabetes, including:

Extra glucose can cross the placenta. Extra glucose triggers the baby's pancreas to make extra insulin. This can cause your baby to grow too large. It can lead to a difficult birth and sometimes the need for a C-section.

Sometimes babies of mothers with gestational diabetes develop low blood sugar (hypoglycemia) shortly after birth. This is because their own insulin production is high.

Babies of mothers who have gestational diabetes have a higher risk of developing obesity and type 2 diabetes later in life.

Untreated gestational diabetes can lead to a baby's death either before or shortly after birth.
also can be caused by gestational diabetes, including:

Symptoms of this condition include high blood pressure, too much protein in the urine, and swelling in the legs and feet

If you had gestational diabetes in one pregnancy, you're more likely to have it again with the next pregnancy.
Diabetes or Diabetes mellitus is diagnosed based on the following criteria
A venous plasma glucose concentration test in done on following parameters
A random venous plasma glucose concentration of 11.1 mmol/L or higher
OR
A fasting plasma glucose concentration of 7.0 mmol/L or higher (whole blood >= 6.1 mmol/L)
OR
An A1C level of 6.5% or higher on two separate tests.
The American Diabetes Association recommends that the following people be screened for diabetes 1:
An important part of managing diabetes — as well as your overall health — is keeping a healthy weight through a healthy diet and exercise plan:
Healthy eating. Your diabetes diet is simply a healthy-eating plan that will help you control your blood sugar. You'll need to focus your diet on more fruits, vegetables, lean proteins and whole grains. These are foods that are high in nutrition and fiber and low in fat and calories. You'll also cut down on saturated fats, refined carbohydrates and sweets. In fact, it's the best eating plan for the entire family. Sugary foods are OK once in a while. They must be counted as part of your meal plan.
Understanding what and how much to eat can be a challenge. A registered dietitian can help you create a meal plan that fits your health goals, food preferences and lifestyle. This will likely include carbohydrate counting, especially if you have type 1 diabetes or use insulin as part of your treatment.
Physical activity. Everyone needs regular aerobic activity. This includes people who have diabetes. Physical activity lowers your blood sugar level by moving sugar into your cells, where it's used for energy. Physical activity also makes your body more sensitive to insulin. That means your body needs less insulin to transport sugar to your cells.
Get your provider's OK to exercise. Then choose activities you enjoy, such as walking, swimming or biking. What's most important is making physical activity part of your daily routine.
Aim for at least 30 minutes or more of moderate physical activity most days of the week, or at least 150 minutes of moderate physical activity a week. Bouts of activity can be a few minutes during the day. If you haven't been active for a while, start slowly and build up slowly. Also avoid sitting for too long. Try to get up and move if you've been sitting for more than 30 minutes.
Treatment for prediabetes usually involves healthy lifestyle choices. These habits can help bring your blood sugar level back to normal. Or it could keep it from rising toward the levels seen in type 2 diabetes. Keeping a healthy weight through exercise and healthy eating can help. Exercising at least 150 minutes a week and losing about 7% of your body weight may prevent or delay type 2 diabetes.
Drugs — such as metformin, statins and high blood pressure medications — may be an option for some people with Prediabetes and other conditions such as heart disease.
Treatment for Type 1 diabetes involves insulin injections or the use of an insulin pump, frequent blood sugar checks, and carbohydrate counting. For some people with type 1 diabetes, pancreas transplant or islet cell transplant may be an option.
Careful blood sugar testing is the only way to make sure that your blood sugar level remains within your target range. People who receive insulin therapy also may choose to monitor their blood sugar levels with a continuous glucose monitor. Although this technology hasn't yet completely replaced the glucose meter, it can lower the number of finger pricks necessary to check blood sugar and provide important information about trends in blood sugar levels.
Besides daily blood sugar monitoring, your provider will likely recommend regular A1C testing to measure your average blood sugar level for the past 2 to 3 months.
Compared with repeated daily blood sugar tests, A1C testing shows better how well your diabetes treatment plan is working overall. A higher A1C level may signal the need for a change in your oral drugs, insulin regimen or meal plan.
People with type 1 diabetes must use insulin to manage blood sugar to survive. Many people with type 2 diabetes or gestational diabetes also need insulin therapy.
Many types of insulin are available, including short-acting (regular insulin), rapid-acting insulin, long-acting insulin and intermediate options. Depending on your needs, your provider may prescribe a mixture of insulin types to use during the day and night.
Insulin can't be taken orally to lower blood sugar because stomach enzymes interfere with insulin's action. Insulin is often injected using a fine needle and syringe or an insulin pen — a device that looks like a large ink pen.
An insulin pump also may be an option. The pump is a device about the size of a small cellphone worn on the outside of your body. A tube connects the reservoir of insulin to a tube (catheter) that's inserted under the skin of your abdomen.
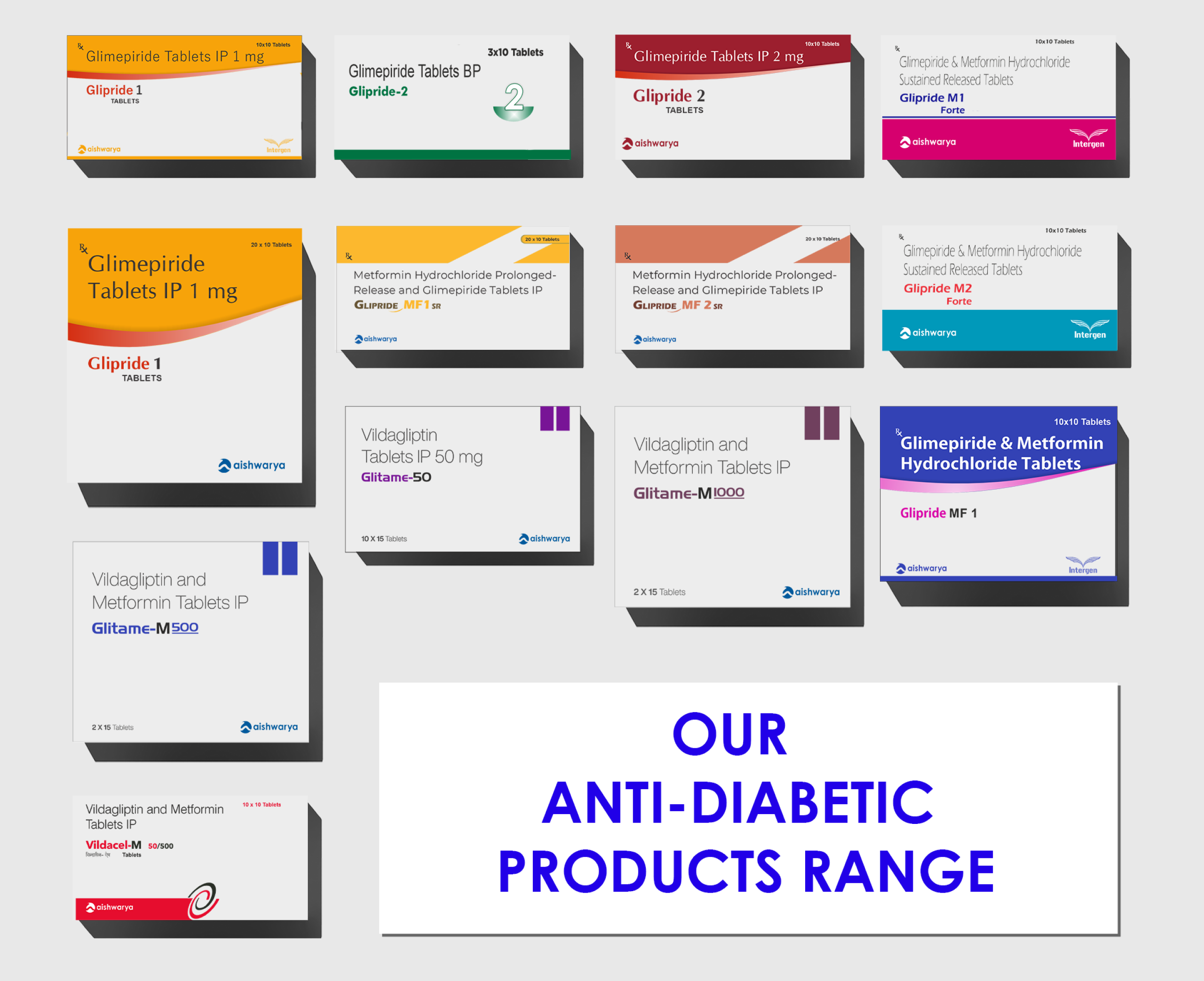
Oral or other drugs Sometimes your provider may prescribe other oral or injected drugs as well. Some diabetes drugs help your pancreas to release more insulin. Others prevent the production and release of glucose from your liver, which means you need less insulin to move sugar into your cells.
Still others block the action of stomach or intestinal enzymes that break down carbohydrates, slowing their absorption, or make your tissues more sensitive to insulin. Metformin (Glumetza, Fortamet, others) is generally the first drug prescribed for type 2 diabetes. Another class of medication called SGLT2 inhibitors may be used. They work by preventing the kidneys from reabsorbing filtered sugar into the blood. Instead, the sugar is eliminated in the urine.
Some common medications used to manage type 2 Diabetes are Biguanides, Sulphonylureas, Alpha glucosidase inhibitor, Thiazolidinediones, DPP-4 inhibitors, SGLT2 inhibitors and Insulin injection.
The use of drug and line of treatment depends on condition of patient and varies accordingly from patient to patient.
Controlling your blood sugar level is essential to keeping your baby healthy. It can also keep you from having complications during delivery. In addition to having a healthy diet and exercising regularly, your treatment plan for gestational diabetes may include monitoring your blood sugar. In some cases, you may also use insulin or oral drugs.
Your provider will monitor your blood sugar level during labor. If your blood sugar rises, your baby may release high levels of insulin. This can lead to low blood sugar right after birth.
Type 1 diabetes can't be prevented. But the healthy lifestyle choices that help treat Prediabetes, type 2 diabetes and gestational diabetes can also help prevent them:

Eat healthy foods: Choose foods lower in fat and calories and higher in fiber. Focus on fruits (before taking discuss with Doctor glycemic index of fruits), vegetables and whole grains. Eat a variety to keep from feeling bored.

Get more physical activity: Try to get about 30 minutes of moderate aerobic activity on most days of the week. Or aim to get at least 150 minutes of moderate aerobic activity a week. For example, take a brisk daily walk. If you can't fit in a long workout, break it up into smaller sessions throughout the day.
Lose excess pounds: If you're overweight, losing even 7% of your body weight can lower the risk of diabetes. For example, if you weigh 200 pounds (90.7 kilograms), losing 14 pounds (6.4 kilograms) can lower the risk of diabetes.
But don't try to lose weight during pregnancy. Talk to your provider about how much weight is healthy for you to gain during pregnancy.
To keep your weight in a healthy range, work on long-term changes to your eating and exercise habits. Remember the benefits of losing weight, such as a healthier heart, more energy and higher self-esteem.
Sometimes drugs are an option. Oral diabetes drugs lower the risk of type 2 diabetes. But healthy lifestyle choices are important. If you have Prediabetes, have your blood sugar checked at least once a year to make sure you haven't developed type 2 diabetes.